What is RCM? Revenue Cycle Management in healthcare is a process of engagement of resources to manage the healthcare practices’ various tasks starting from patient appointment scheduling, updating patient demographic and active coverage records in the EHR/Practice Management System, providing healthcare services, updating patient charts in EHR, transmitting claims to insurance carriers and patients, maintaining all healthcare industry requirements up until getting the medical claims finally paid either by insurance companies, patient or third party processor whichever is applicable. During the process of RCM, medical billing, or practice management software can be utilized and integrated with a healthcare clearinghouse along with certified EHR (electronic health record) or EMR (electronic medical record) and an automated patient portal to streamline the process and improve the overall patient experience at the healthcare office.
Healthcare RCM simplifies the business process and improves the clinical sides of the healthcare sector by maintaining the administrative data, such as a patient’s name, insurance carrier details, clinical data such as procedure and diagnosis, along with complete medical treatment history, the transmission of data over the EDI (electronic data interchange) through clearinghouses to achieve the goal of getting the reimbursement from insurance carriers and patients in a timely fashion. Medical billing companies like iCareBilling offers RCM Process workflow improvement to help healthcare providers achieve their goals to improve patient care.

Coordinating with insurance carriers is a fundamental part of the Revenue Cycle Management Services (RCM). When an appointment is scheduled at the healthcare office, the doctor’s office intake department generally verifies the patient’s insurance details if the patient has active coverage before the actual visit date to ensure the accuracy of insurance data. After an insurance-covered patient receives the treatment for their relevant diagnosis and paid any applicable copays, a medical professional or medical coder analyzes the nature of the treatment provided in accordance with the international classification of diseases (ICD-10 codes) and assigns the relevant codes. The medical billing department of a healthcare facility or in case of having an outsourced Healthcare RCM Services provider, Medical Billing Companies then send the patient’s treatment, diagnosis, and date of service, along with the patient and healthcare provider required information to the patient’s insurance company to get the maximum reimbursement that can be covered by the insurance. Based on the mutual agreement between the patient and insurance, some portion of the medical claim might be covered by the patient such as co-insurance, deductible, or in some cases the treatment that is not covered under the patient plan, and all such patient responsibilities are then being billed to the patient if they have not paid upfront. Depending on the specialty of the healthcare facility, or provider specialty, and the patient’s insurance plan sometimes patient responsibility can be determined before even providing services which will result in the reduction of expenses that occur for patient billing that includes mailing out paper statements and/or e-statements or in some cases text message or phone call reminder but it also enhances the overall RCM Services for the practice because full payment on the claim can be made with less time so no more following up patients.
RCM or Revenue Cycle Management
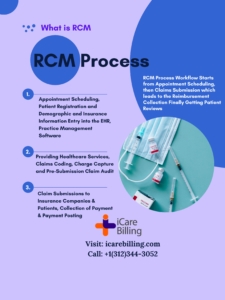
The Best Healthcare RCM Companies always focus on developing the RCM Process to ensure result-oriented and quality service delivery. The RCM or revenue cycle management involves the process related to all the clinical and administrative aspects of the healthcare business that will include collection and management of patient clinical and non-clinical data, charge capture or generally called charge posting, and ensuring the accurate healthcare claims data management, handling rejection and denials, payment posting or electronic funds transfer (EFT) management, account receivable follow-up and denial management. Medical billing companies have separate EDI Enrollment departments to help streamline the whole process to make it easier for healthcare providers.
Here is what’s involved in the revenue cycle management process:
- Pre-Registration before Visit: Collection of patient information before the actual visit date, patient name, date of birth, address, phone, email, and active insurance coverage details, before a patient arrives for outpatient or inpatient services at the healthcare office.
- Registration a the time of Visit: Collection of necessary information related to the previous history, any referral or prior authorization in case of being seen by a specialist or surgeon, or others, and collection of other necessary information to establish a medical record and to meet various healthcare regulatory and industry clinical requirements.
- Charge Posting: Providing healthcare services to patients and converting them into billable claims
- Medical claims transmission: Submission of healthcare claims with an appropriate fee schedule to the insurance companies, and others.
- Medical Coding: Conversion of patient chart notes into the ICD-10 diagnosis codes, procedure codes, modifiers, units, etc.
- Patient Payment Collections: Identifying the patient balances and collecting the patient payments.
- Electronic and Paper Remittance Processing: Working on denied claims and taking appropriate actions and applying the payments into the practice management software to settle the claim or to bill the patient for patient responsibilities.
- Denial Management and Claims Follow-up: Following up on unpaid claims that cross a certain threshold and payments have not been received either electronically or via paper mail EOB (Explanation of Benefits) to ensure and resolve denied claims for possible resolution to get the reimbursement.
- Audit Review: Auditing the Healthcare RCM process to ensure the highest accuracy and maintain all industry requirements.
Revenue Cycle Management Process and Factors:
RCM Services offered in healthcare by a medical billing company are directly connected with financial matters and there are a few factors (internal and external) that directly impact revenue cycle management and collection.
A healthcare entity can be flexible with administrative control over internal dynamics, such as healthcare provider productivity, new and established patient volume, and fees for services (FFS). However, it is more challenging to make an impact on external factors, such as patient insurance payments or claims reviews and denials from insurance companies. Even though we at iCareBilling believe that somehow external factors can also be influenced by talking to the insurance and raising the issue to the level where it could get some solution or adopt more compliant practices to reduce denials and improve collections at healthcare offices. It’s an important part of Medical Billing Services to provide such valuable inputs to healthcare providers.
RCM or Revenue Cycle Management Systems
Medical providers often purchase and deploy designated RCM (revenue cycle management) systems to store and manage patients’ clinical and non-clinical records. An effective Revenue Cycle Malmanagement (RCM) system can reduce the amount of time spent while delivering medical and related services and receiving payment by interacting with other healthcare IT systems — such as EHR (electronic health record) or EMR (electronic medical record) (EHR) and/and practice management/medical billing systems — as patients move through the care process.
An effective healthcare RCM system can also save healthcare staff time by automating the medical billing and other clinical processes that were previously handled by employees. These tasks include administrative tasks, such as coordinating with patients regarding their upcoming appointments, reminding patients about their due balances, sending balance statements on time, enhancing EDI (electronic data interchange) capabilities between EHR / Practice Management System and the clearinghouse to fetch the data from insurance companies, and having an audit review system in place to identify and fi the denied claims and have the team work on them to fix the errors/issues.
Revenue Cycle Management Systems offered by a medical billing company can help healthcare providers to save a lot of financial resources by giving having a good designed RCM Process in place to automate patient appointment scheduling, patient intake entry, clean claim submission, and getting the desired reimbursement. We have learned throughout the years that if you have specialty-focused RCM Services, or medical billing services in place, that can help you not only comply with your specialty healthcare and regulatory requirements, it gives you a better insight into patient experiences, analyze key performance indicators at the patient treatment level as well as employee’s productivity and this refines the overall patient experience and improve the care standards within the specialty and overall, in the healthcare industry.
